Department Research Areas
Musculoskeletal Biomechanics and Rehabilitation Engineering
Musculoskeletal biomechanics and rehabilitation engineering are interconnected fields within biomedical engineering that focus on understanding the mechanics of the musculoskeletal system and developing technologies to improve mobility, function, and quality of life for individuals with physical impairments. Musculoskeletal biomechanics studies the mechanical behavior of the human body’s musculoskeletal system, including bones, muscles, tendons, ligaments, and joints. It applies principles of physics, mechanics, and biology to understand how forces interact with these structures during movement and physical activity.
Rehabilitation engineering focuses on designing devices, systems, and technologies to assist individuals with disabilities or injuries in regaining mobility, independence, and functionality. Musculoskeletal biomechanics provides the foundational knowledge needed to understand the mechanical aspects of movement and injury, while rehabilitation engineering applies this knowledge to create practical solutions for restoring function. Together, these fields aim to enhance human mobility and improve quality of life for individuals facing physical challenges.
Participating Faculty
The following faculty work on research around musculoskeletal biomechanics and rehabilitation engineering. Visit their profile pages to learn more about their specific areas of research.
Sample Projects
Anteriorly Stabilized Total Knee Arthroplasty
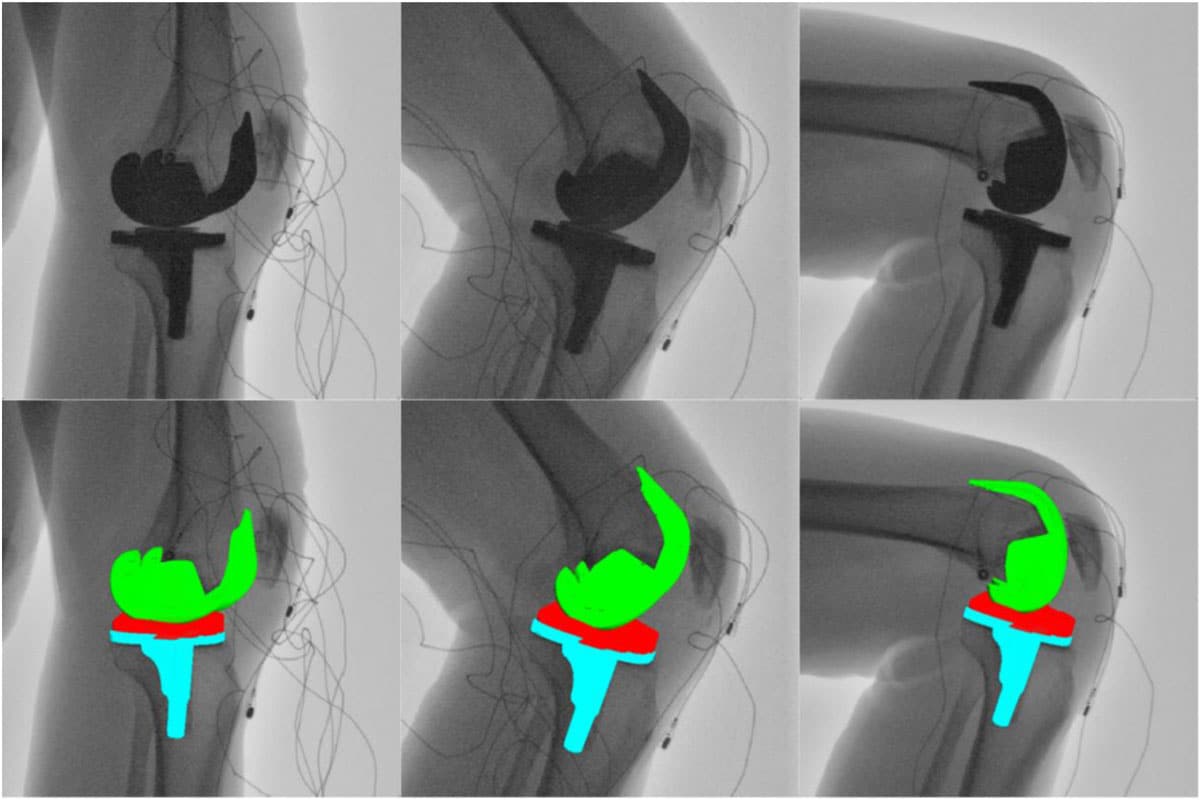
Total Knee Arthroplasty (TKA) involves the replacement of damaged bone and cartilage within the knee joint to alleviate joint pain and restore overall function to the patient. Unfortunately, to properly expose the joint during surgery and to create space in the knee for the components themselves, surgeons must resect key stabilizing soft tissues within the joint, notably the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL). With these stabilizing structures removed, the implanted knee is subject to instability and paradoxical sliding.
The University of Tennessee’s Center for Musculoskeletal Research is working with industry-leading orthopaedic companies to design mechanical constraints to replace the functionality of these key ligaments. Notably, a novel TKA design, the “Bi-Cruciate Stabilized” TKA, incorporates a unique cam-and-post mechanism that strives to replicate the constraints that the ACL and PCL provide. The effectiveness of these design features is still under investigation, but early in vivo fluoroscopic studies demonstrate stable overall kinematics during both flexion and extension-based activities, indicating a promising future for stable TKA.
Representative publications:
LaCour MT, Smith LA, Cates HE, Tim-yun Ong M, Shu-hang Yung P, Komistek RD. The effects of anterior stabilization in Bi-cruciate stabilized and posterior stabilized total knee arthroplasty during a weight-bearing extension activity. The Knee, Volume 56 (2025). https://doi.org/10.1016/j.knee.2025.06.024.
Biomechanics of Artificial Tendon
At least 4% of all musculoskeletal injuries involve tendons and ligaments. Large tendon defects that cannot be repaired directly are especially devastating. The gold standard for repairing large tendon defects is to bridge the gap with a graft taken from another healthy tendon of the same patient. This may cause disability at the donor site. There is an urgent need for artificial devices and materials that can be used to repair or replace damaged tendons. In collaboration with the UT College of Veterinary Medicine, our lab develops and tests artificial tendons and grafts for replacing part or all of a damaged tendon. In some tests, the artificial tendons were tested in an animal model by surgically implanting it in place of a biological tendon, then measuring the motion and forces of the affected limb while the animal moved. Results from these studies could one day improve the function of patients with tendon injuries.
Representative publications:
Fidelis OP, Easton KL, Smith M, Bastos G, Bowers K, Anderson DE, Crouch DL. Replacing biological Achilles tendon with polyester silicone-coated artificial tendon: effect on rabbit hindlimb movement biomechanics and muscle morphology. Biomechanics, 5(3), 47; https://doi.org/10.3390/biomechanics5030047.
Easton KL, Hatch C, Stephens K, Marler D, Fidelis O, Sun X, Bowers KM, Billings C, Greenacre CB, Anderson DE, Crouch DL. Replacement of tibialis cranialis tendon with polyester, silicone-coated artificial tendon preserves biomechanical function in rabbits compared to tendon excision only. Journal of Orthopaedic Surgery and Research, 19, 2024. https://doi.org/10.1186/s13018-024-04581-7
Shoulder Exoskeleton Biomechanics
Elevating the shoulder against gravity is critical for performing tasks needed for independent living and manual work. Shoulder elevation may be difficult or limited in patients with shoulder disability due to musculoskeletal injuries, such as rotator cuff tear, and neurological disorders, such as stroke. Workers who elevate the shoulder to perform overhead tasks have a high risk of developing a shoulder injury. There is a need for wearable assistive devices, such as exoskeletons, that can help people elevate the shoulder to overcome disability or reduce injury risk. Our lab measures the biomechanical effects of shoulder exoskeletons to better understand their benefits and potential risks.

Representative publication:
Asgari M, Phillips E, Dalton BM, Rudl JL, Crouch DL. Design and Preliminary Evaluation of a Wearable Passive Cam-Based Shoulder Exoskeleton. ASME Journal of Biomechanical Engineering. 144(11): 111002 (12 pages), 2022. https://doi.org/10.1115/1.4054639.
Hall PT, Crouch DL. Effect of Continuous, Mechanically Passive, Anti-Gravity Assistance on Kinematics and Muscle Activity During Dynamic Shoulder Elevation. Journal of Biomechanics, 103, 2020. https://doi.org/10.1016/j.jbiomech.2020.109685.
Nelson AJ, Hall PT, Saul KR, Crouch DL. Effect of a Wearable Mechanically Passive Shoulder Exoskeleton on Muscle Activity: A Computational Simulation Study. Journal of Applied Biomechanics, 36(2): 59-67, 2020. https://doi.org/10.1123/jab.2018-0369.
